First described over 250 years ago, was known as Jeep disease during WWII. Nearly 80000 soldiers were treated for this condition during WWII!.
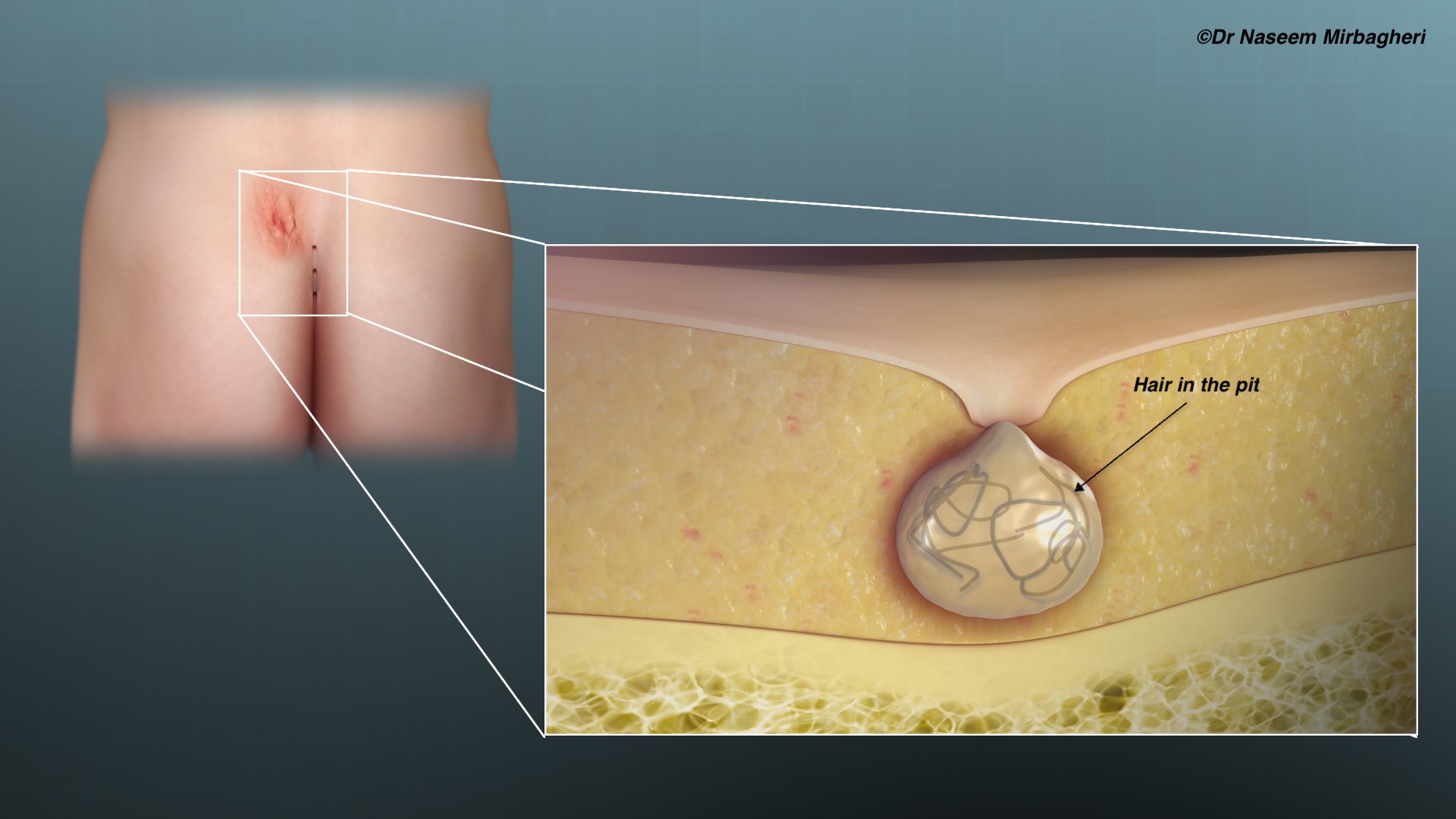
Pilonidal comes from the Greek work and means ‘nest of hair’
It is a rare disease in patients <12yo and >40yo. Risk factors include race, occupation, male gender, family history, deep natal cleft, poor hygiene, hairiness and obesity.
It is actually a dermatological condition caused by swollen hair follicles in the natal cleft (can be in other parts of the body too), these follicles can be invaded by hair (from buttocks, neck etc) which can result in chronic inflammation and sometimes an abscess when the hole or ‘pit/sinus’ becomes completely blocked by hair. It is thought to be an acquired condition, therefore you are unlikely to be ‘born with it.
If you have been diagnosed with the disease and have no symptoms at all e.g., discharge, swelling or pain, then you can successfully manage it by hair control e.g., laser hair removal of the buttocks, try and avoiding shaving.
If you have the disease and have had one infection/abscess and have no interval symptoms (i.e., completely symptom-free after the abscess drainage), you can also consider hair control measures only but at higher risk of another infection than those who have never had any infection.
If you have the disease and have recurrent infection and/or ongoing symptoms then there are few surgical options available to you depending on the severity of disease, the number of pits etc. and the experience of the surgeon you visit.

These options may include any of the following:
- Destruction of the sinus e.g. with phenol
- Minimally invasive surgery e.g. sinus-ectomy (removal of the pit or sinus only)
- Excision of all the disease with either wound being left open or closed with sutures e.g. Karydakis
- Various flap procedures e.g. Rhomboid flap
The recurrence rate of pilonidal sinus can be up to 20 % with less aggressive surgeries and with flaps up to 10%.
REMEMBER the natal cleft area has a very poor healing capacity and most invasive surgeries will result in wound breakdown and infection, requiring dressings and wound care for up to 6months.
SOMETIMES, the treatment may be worse than the disease itself, so when considering major invasive surgery such as flaps or karydakis, always assess how bad your disease is, how much does it bother you on daily basis and ensure you have enough social support for the postoperative phase of wound healing.
You must make any treatment choices in consultation with your treating surgeon and your local doctor.
REMEMBER this is a benign disease, there is a very small handful of case reports reporting cancer formation in pilonidal disease. It is likely to be in cases where there is severe chronic inflammation over many years. We do NOT treat this condition as a premalignant disease, so you can rest assured.

