
What is diverticular disease?
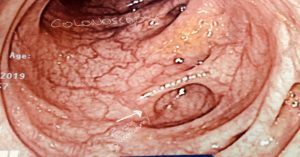
Diverticular disease refers to the little pockets or pouches that form in the bowel usually from the weakening of the bowel wall. This condition is mainly seen in the sigmoid colon (large bowel on the left side). This condition is very common in Australia and commonly found incidentally during a routine colonoscopy in patients age 45 or above (30-60% risk). Risk factors for developing this condition is low fibre diet, chronic constipation, genetics and ageing. These pouches in the colon are weak ares and can lead to complications such as bleeding and perforation. Majority of patients have NO symptoms from this condition and will need NO treatment.
Common terms to know about when referring to diverticular disease and its potential complications:
Diverticulosis : when you have this disease with NO symptoms
Diverticulitis: when you have infection in one or more of these pockets leading to pain, majority of these patients will respond to oral antibiotics. In more severe conditions especially when one of these infected pockets bursts or perforates, you will need hospital admission and rarely emergency surgery. If you have this problems you will feel unwell and have severe abdominal pain.
Diverticular bleeding: one of the most common causes of painless bleeding from the back-passage. More than 90% of patients with bleeding from diverticular disease will settle with no intervention, some may need a radiological intervention to stop the bleeding. Surgery is rarely needed.
Diverticular perforation: refers to the bursting of a diverticulum or pouch, this can be a catastrophic event for some, especially when the perforation is ‘free’ and faeces or pus spreads throughout the abdomen. In such scenarios, a person will present with sudden pain in the abdomen that is unrelenting, they may have a temperature, be nauseous and feel unwell.
Diverticular abscess: a pocket of pus that collects around your bowel when one of these diverticulum or pouches bursts, lucky for some people the perforation is not ‘free’ and is contained by the fat or the ‘omentum’ inside the abdomen forming an abscess. In most circumstances, this collection of pus can managed with antibiotics or drainage via a small cut through the skin under guidance of a CT scan. If these measures don’t work, then surgery maybe required.
Diverticular fistula: This is where long-term inflammation in the bowel can ‘erode’ into adjacent structures and form a communication. Most common is in the bladder also known as colovesical fistula. Patients with colovesical fistula may have symptoms of passing air via the bladder when urinating known as ‘pneumaturia’ or more commonly with recurrent urinary tract infection. In women, especially after hysterectomy, fistulisation to the vagina can occur (colovaginal fistula). In such cases, one can present with passage of air or faeces per vagina. All patients with fistulisation to the vagina or bladder will need surgery.
Diverticular stricture: chronic inflammation in the bowel can result in narrowing, someone with diverticular stricture can present acutely with a large bowel obstruction or more gradually over time with difficulty opening bowel, bloating and worsening constipation. Surgery is usually required for this condition.
Management of diverticular disease:
Majority of patients with diverticular disease have no symptoms and will need no treatment. Once you have the disease, it cannot be reversed. Maintaining a healthy diet with high fibre and avoiding constipation are your best chances of avoiding more diverticulum forming.
Patients with infections can usually managed with antibiotic either in hospital or as outpatient.
Patients with free perforation will need surgery – a procedure called Hartmann’s is usually performed in such circumstances, this is where the diseased segment of your bowel (usually the sigmoid) is removed and a stoma (colostomy or a ‘poo bag’) is created. Depending on the skills of your surgeon, a variation of this surgery can be performed (high anterior resection), regardless of the type of surgery, some type of stoma is usually fashioned.
In all other circumstances ( e.g. diverticular fistula, stricture or where you have recurrent diverticulitis) where there is no contamination and you are fit, a high anterior resection (either laparoscopic or open) is performed.
If you have any of the above symptoms or are concerned about your bowels, please visit your GP to discuss your symptoms.

